Help! Does My Kid Really Have ADHD?
/It’s the start of a new school year, which inevitably means I will begin getting calls from parents left and right with the infamous question, “My child’s teacher is saying he/she has ADHD, can you help?” I want to start by saying that Attention-Deficit/Hyperactivity Disorder (ADHD) is a very real diagnosis and I will always do my due diligence to evaluate for the symptoms, but I’m also a natural skeptic and am not the kind of therapist who is going to hear that a child is hyper or has a hard time focusing and immediately diagnose ADHD. The fact is there are several diagnoses that have overlapping symptoms and I personally make it a priority to rule these out before jumping to ADHD.
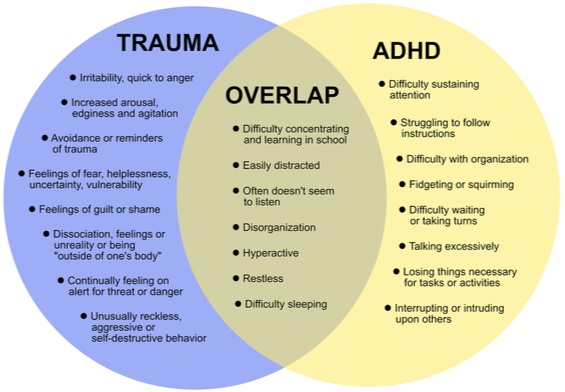
One misdiagnosis I am especially sensitive to is Child Traumatic Stress vs. ADHD. After working with childhood trauma for several years, I have met with many kids who had previously been diagnosed ADHD before there was a known trauma, only to find they had been traumatized or encountered an abusive situation around the same time the ADHD symptoms showed up. That being said, I also encountered several clients who had experienced trauma and were also appropriately diagnosed ADHD. The kids’ behaviors appear to be similar, but what I found is that the trauma clients who had hyperactive symptoms or difficulty focusing were reacting to trauma triggers, and as we began to work through the trauma and introduce coping skills, their hyperactive symptoms decreased. In the kids I saw who were traumatized and diagnosed ADHD, there was definitely a decrease in their symptoms, but they would still become frustrated about not being able to pay attention, have difficulty learning and have a hard time sitting still, even without the presence of a trauma trigger or reminder.
For visual reference, check out this diagram below:
Source: https://www.nctsn.org/sites/default/files/resources//is_it_adhd_or_child_traumatic_stress.pdf
So again, I say, there is definitely a difference between trauma and ADHD, but a lot of times they can look the same, especially to teachers (or even parents) who may be unaware of a trauma or other disorder. In counseling, I frequently talk to parents about “Big T Traumas” and “little t traumas” to differentiate between diagnosable (T)rauma that often leads to Post Traumatic Stress Disorder (direct exposure to or witnessing abuse, neglect, catastrophe, war, or violence) and impactful life event (t)raumas that can lead to similar symptoms (bullying, moving houses/schools, the birth of a sibling, death of a close family member or friend, etc.). This isn’t meant to minimize the impact of any event in a child or adult’s life, but to help parents, kids, and adults understand that we can exhibit trauma symptoms even if there wasn’t the experience of what we sometimes assume trauma to be, i.e. abuse, neglect, violence, etc.
You might be thinking, that’s all good and fine, but what does any of this mean and what should I do about it? Well, lucky for you, I’m going to break it down into bullet points because everything I’ve read about blogging says that people only read the first 100 words of an article and then skim for pictures and headings…so if you made it this far, congratulations, and thanks for hanging in there!
Here’s four things to consider if your child’s teacher thinks your child may be ADHD:
Know That ADHD is Real and Not a Made-Up Diagnosis
In recent years, I have been fairly surprised because once people learn that I’m a therapist, one of the first questions they ask (after “So are you psychoanalyzing me right now?”) is “Do you think ADHD is a real thing?” A lot of times I giggle to myself because I can’t help but feel like they’re asking me about some decades-old folklore like Big Foot or the Loch Ness monster. The truth is, ADHD isn’t something I discovered or undiscovered, but, in recent years, has gotten a lot of bad rap after a wave of over-diagnosing and over-medicating. I think it’s time to call a spade a spade: ADHD isn’t something that is made up or should be used to unneccesarily put a hyper child on medication, but it is a real diagnosis that a lot of kids struggle with and often need medication to manage the symptoms.
If Your Child’s Teacher Suggests ADHD, Take it Seriously
In light of my last point, please don’t immediately write off your child’s teacher if they suggest your child might have ADHD. Like I said, ADHD is a real thing, and if a teacher is bringing it up, chances are they are seeing a behavior or multiple behaviors they are worried about. They work with kids all day every day and I trust can tell the difference between normal child behavior and development versus concerning behavior. As a parent, if a teacher brings this to your attention, I encourage you to do your due diligence and consult with your child’s pediatrician and/or a child therapist for further evaluation. They can thoroughly assess for ADHD symptoms, as well as symptoms of other diagnoses, including anxiety, depression, trauma, etc.
Be Aware That Trauma and Other Diagnoses are Also Possibilities
If your child has been in school for several years and has never had difficulty focusing, sitting still, or learning and then begins acting out of the ordinary, don’t immediately jump to conclusions, but trust your gut and know that you know your child better than anyone. It can help to backtrack and think about possible big life events or stressors the child has recently experienced. If you’re worried, it doesn’t hurt to talk to your child; tell them you’ve noticed them acting different, and check-in to see if they have noticed their behavior or feelings change as well. Again, this doesn’t immediately mean “Big T Trauma,” but may be an indication that something changed or is impacting them.
Consult With a Professional and be Curious
If you’re really not sure what is going on, it’s in your best interest to reach out to an experienced therapist or doctor. Don’t be afraid to be skeptical and ask questions:
How do you typically work with hyperactive kids?
How do you differentiate between ADHD and other diagnoses?
What are your beliefs about medication for children?
Do you have experience working with childhood trauma and do you know the difference?
How involved are parents in the therapy process?
You are the parent and have to do what is in the best interest for your child. A part of this is finding a therapist who fits; someone who works well with you and your child; someone who is professional, but also makes your child comfortable; someone who advocates for your child and is on their side; someone who knows how to talk with parents and is willing to involve the parents in the process (especially for younger children); and someone who is patient and doesn’t force your child to open up sooner than they are ready. We want our kids to be kids and whether they are struggling with ADHD or another diagnosis that’s impacting their everyday life, we want to help them be happy, healthy and free to enjoy their childhood with as few disruptions as possible.
I call this “ADHD season” because kids inevitably get through summer without any problems; they’re outside or inside playing, there isn’t a rigid structure, they’re with friends or family, going on vacation, etc., but a lot of times when the school year starts is when the symptoms become more apparent. With the immediate adjustment to structure, learning, rules, expectations, etc., it’s not uncommon for therapists to get more calls around this time of year for children struggling to pay attention or behave well in the school environment. I’ve found there are several reasons for this; some being ADHD, other being bullying, or sometimes even a (T)rauma or (t)rauma, but it never hurts to ask for help or seek out a professionals opinion.